When Bloom recalls the death of his infant son in Calypso,
he twice thinks that the experienced midwife ("Lots of babies
she must have helped into the world") could tell at once that
the infant would not survive: "She knew from the first poor
little Rudy wouldn't live. Well, God is good, sir. She knew at
once." How, one wonders, could she have known that? And can
readers share in her omniscience by learning what killed Rudy?
Two chapters later, the novel offers a clue to the first
question: Rudy's skin looked purple. With no diagnostic
testing or autopsy having been performed, the second question
cannot be answered definitively. But the addition of another
clue—in Ithaca, we learn that Rudy died eleven days
after birth—suggests that he may have died of a congenital
cardiac defect known as Hypoplastic Left Heart Syndrome
(HLHS).
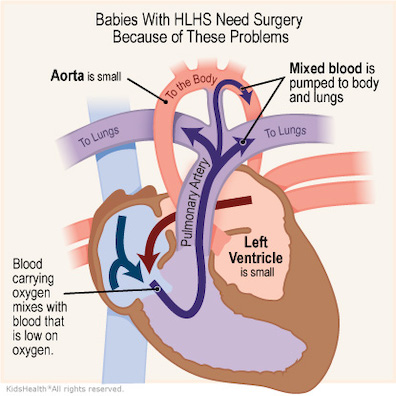
HLHS is characterized by a severely underdeveloped left
ventricle and ascending aorta, and by the presence of a septal
defect allowing blood to flow between the two atrial chambers.
In a normal heart, blood that has flowed from the right
ventricle to the lungs to take in oxygen returns to the left
atrium and moves from there to the left ventricle, which pumps
it through the aorta to the rest of the body. In the abnormal
development of HLHS the left ventricle is too small to pump
oxygenated blood to the body (in the worst cases, only a
slit), and the ascending aorta is likewise diminutive (in the
worst cases, only a thread).
With its normal passage blocked, the oxygenated blood in the
left atrium passes through the atrial septal defect always
found in cases of HLHS into the right atrium and thence into
the right ventricle, where it mixes with the oxygen-poor blood
that the veins have brought back to the heart from the body.
The pulmonary artery carries some of this mixed blood (shown
as purple in the illustrations) to the lungs, but some of it
passes to the rest of the body via the ductus arteriosus, a
fetal blood vessel connecting the pulmonary artery and the
aorta that, in utero, lets most of the blood bypass the
fluid-filled, not-yet-functioning lungs of the fetus. In
healthy babies the ductus arteriosus closes shortly after
birth.
As long as the fetus with a hypoplastic left ventricle
remains in the womb it is sustained by the oxygen it receives
from the mother's blood. As soon as the umbilical connection
is severed, however, the baby must depend solely on the poorly
oxygenated blood pumped from its right ventricle. Oxygen
saturation plummets to about 85%, resulting in marked cyanosis
(purplish skin). The decreased oxygenation delays the closure
of the ductus arteriosus, allowing adequate blood flow to the
body for a short while, but eventually this vessel does
close—typically in about 11 days. Blood flow is greatly
reduced, and death follows quickly. Without treatment, HLHS is
universally fatal.
The precise birth and death dates detailed in Ithaca
provide one indication that Rudy may have died from HLHS or
some other "ductal-dependent lesion" revealed by the closing
of the ductus: "birth on 29 December 1893 of second (and only
male) issue, deceased 9 January 1894, aged 11 days."
Another clue comes in Hades when Bloom sees a child's
tiny coffin and is reminded of his little boy's cyanotic
appearance: "A dwarf's face, mauve and wrinkled like
little Rudy's was. Dwarf's body, weak as putty, in a
whitelined deal box." Although the illustrations here
exaggerate the red color of oxygenated blood, the blue color
of venous blood, and the purple color of their mixing, the
three kinds of blood do display these distinctive colors. The
narrative itself exaggerates the cyanosis of Rudy's skin by
describing it as mauve, a rich
purple hue. The purple coloration must have been the trigger
for Mrs. Thornton's intuitive judgment that the baby was
suffering from a fatal condition.
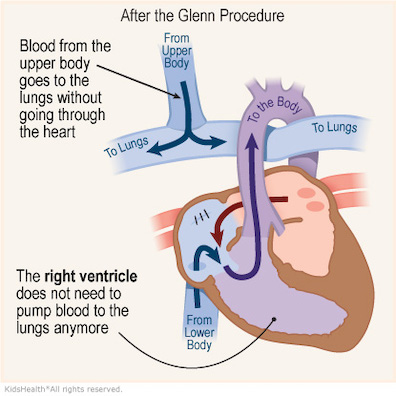
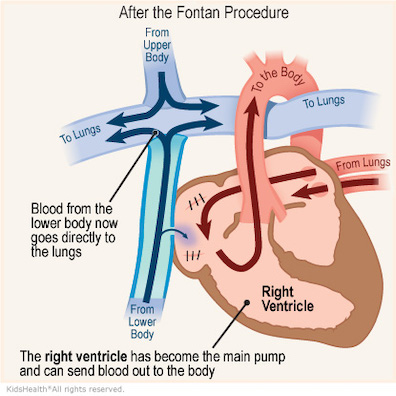
Today, there are three staged surgical procedures for
rebuilding these infants' malformed hearts: the multifaceted
Norwood procedure, generally performed in the first week of
life and fatal more than 10% of the time; the Glenn procedure
(Bidirectional Glenn Anastomosis),
usually done at about six months of age and carrying a much
lower surgical mortality risk of 1-3%; and the Fontan
Procedure, performed at 18-24 months with a comparably low
risk of death. The three operations are performed
successively, each building on the work of the former. They
are palliative, not curative, leaving the child with only a
single functioning ventricle.
Even with surgical and medical interventions, mortality and
morbidity from HLHS remain high. Children with the condition
typically suffer from incomplete brain development during
gestation and score in the low-normal range on IQ tests; other
somatic complications are commonplace. One study showed that,
a year after the Norwood Procedure, the mortality rate was
25%. Over time, survival rates increase. For children who
survive to the age of 12 months, long-term survival up to 18
years of age is approximately 90%. Even had the Blooms been
able to take advantage of these open-heart surgeries, their
lives as parents would not have been easy. But the development
of the three procedures lay many decades in the future. In
1904, HLHS was a death sentence.
Surrounded by large families, Joyce may have known of
infants who died at about 11 days of age, or his brief stints
as a medical student in Dublin and Paris could have
familiarized him with the deadly heart condition. Although
rare, HLHS is common enough to be known to all doctors: in the
U.S. the prevalence is approximately 2-3 cases per 10,000 live
births. HLHS accounts for 2-3% percent of all cases of
congenital heart disease and afflicts males approximately 1.5
times as often as females.